Reliance Matrix
Rebuilding a legacy disability claims platform to improve clarity, compliance, and employee confidence
Reliance Matrix initiated a digital transformation effort to replace a legacy disability claims portal that lacked transparency and usability.
Employers struggled to interpret complex claim data, and employees had little visibility into their own benefit timelines. Many relied on HR to understand when a claim began, when it ended, and how payments were calculated. Information was often surfaced through static exports that were difficult to interpret and not actionable.
The objective was to create a clearer, modernized experience that provided real-time insight into claims while improving compliance, operational efficiency, and employee confidence.
Legacy Portal Replacement
Claims Workflow Redesign
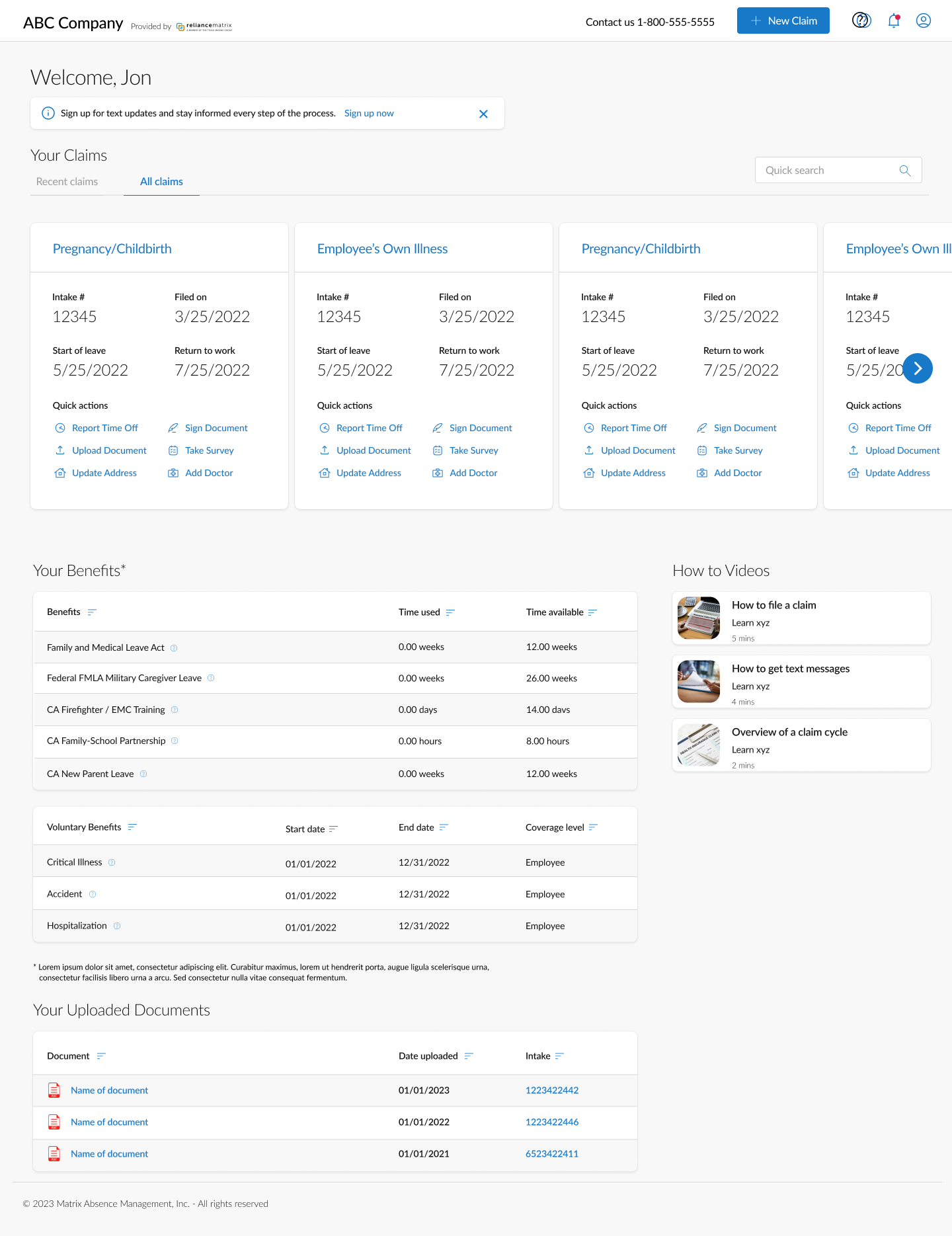
Employee Self-Service Experience
Information Architecture & Data Clarity
UX & UI System Modernization
Compliance-Aware Interaction Design
Scope
Role & Ownership
DodgeUX served as the design lead and strategic UX partner throughout the engagement, operating in an embedded capacity alongside product, engineering, and compliance teams.
We directed overall workflow restructuring, defined new interaction models, and led system-level experience decisions across both employer administrative and employee-facing views. Working sessions were facilitated to clarify requirements, identify friction points, and align on regulatory constraints before iterating through multiple design refinements.
The focus was on shaping a clear, compliant, end-to-end claims experience rather than simply refreshing the visual layer.
The Real Problem
The legacy claims portal lacked transparency and clarity in a highly regulated environment. Employees struggled to trust the information presented to them, often relying on static PDFs or HR intermediaries to understand their claim status, payment amounts, and benefit timelines.
Disability coverage rules varied by state and federal requirements, creating layered complexity across payout phases and eligibility periods. However, the system did not clearly communicate these distinctions. Claim names were difficult to interpret, timelines were unclear, and payment breakdowns lacked contextual explanation.
For employers, visibility was limited and fragmented. Administrative tools did not provide a cohesive view into employee claims, documentation, or reporting needs. In a domain where accuracy, compliance, and trust are critical, the experience created confusion rather than confidence.
What Changed / Outcome
The redesigned platform introduced structured clarity into a previously opaque process.
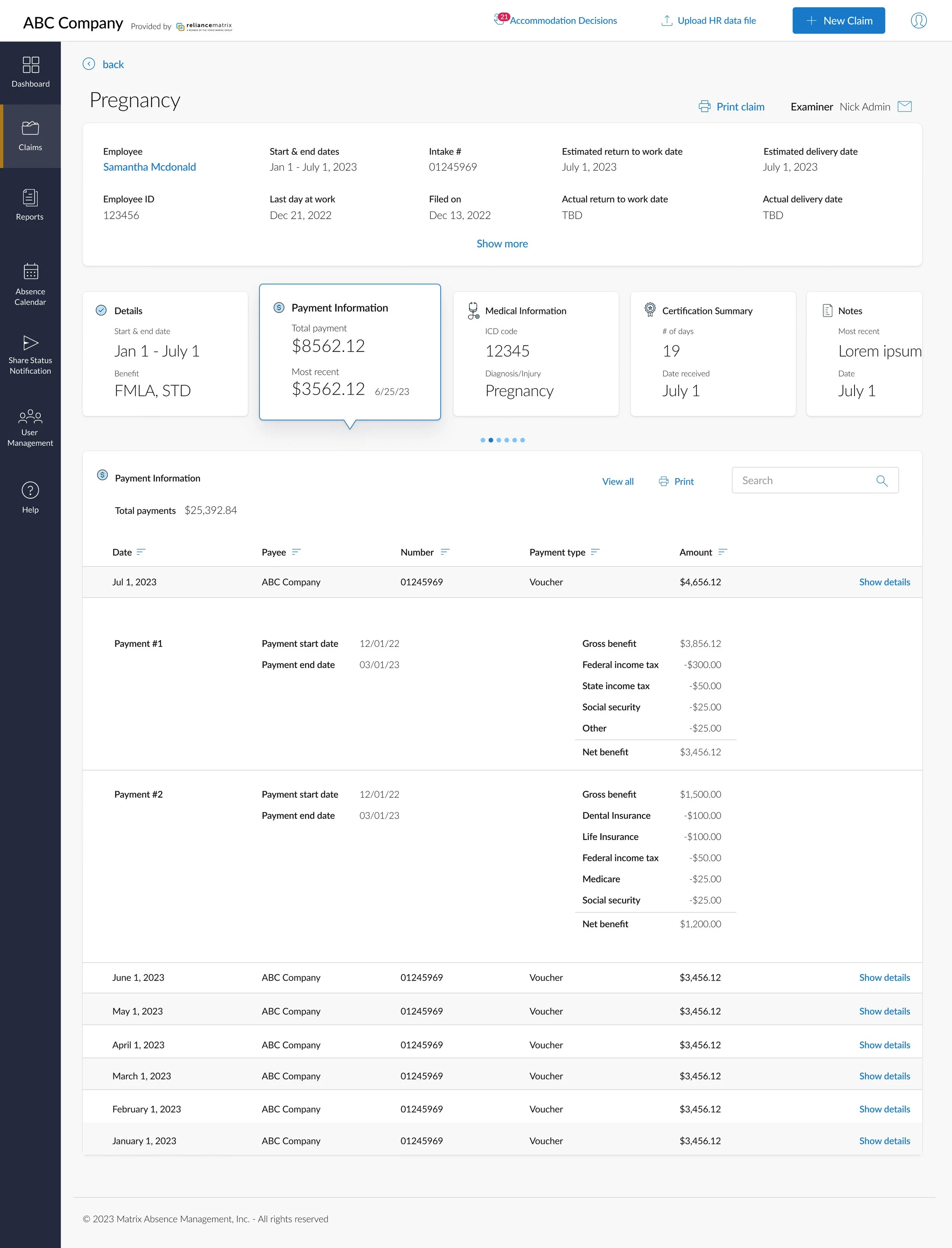
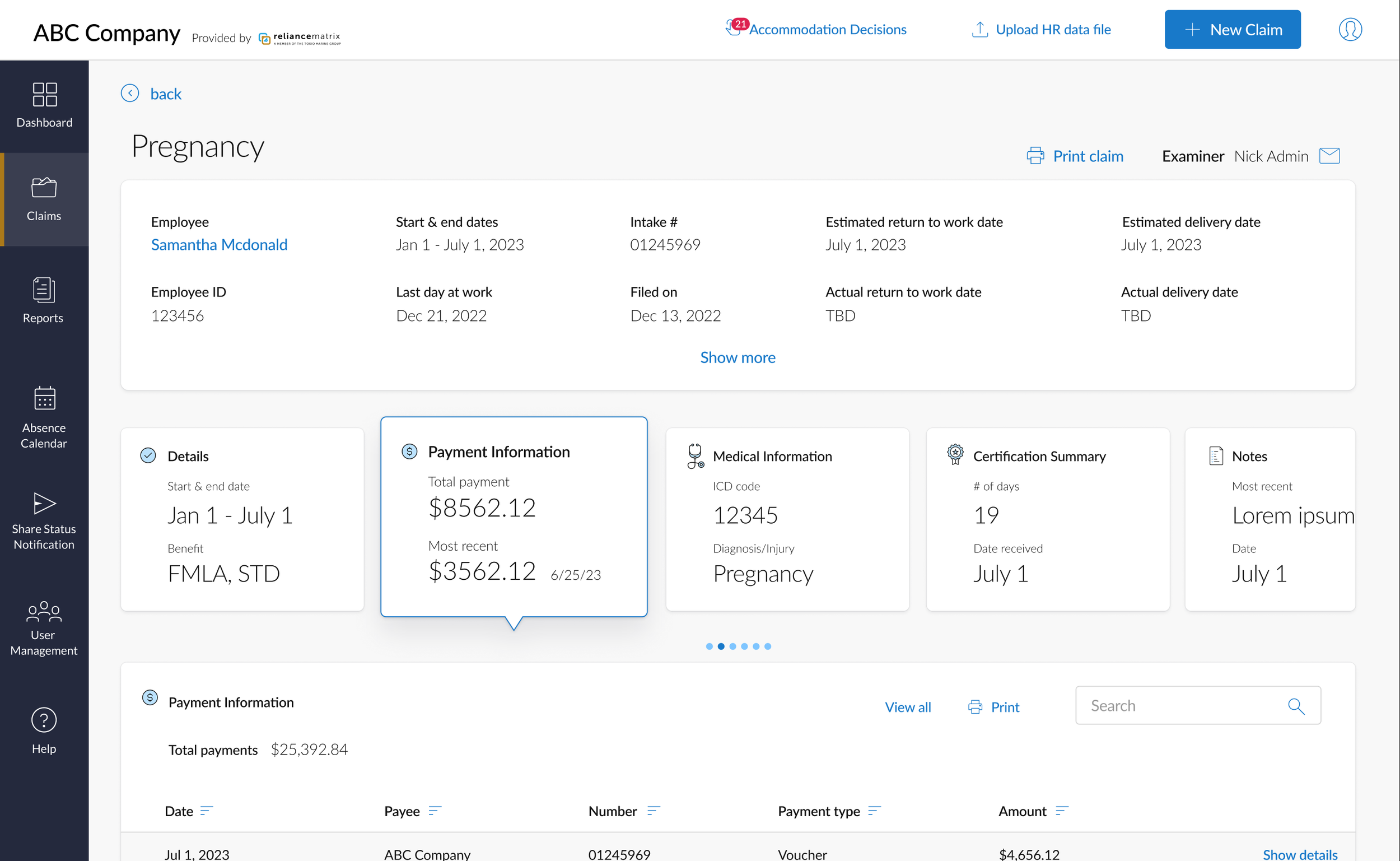
Interactive timeline visualizations helped employees understand when claims began, when phases shifted, and how federal and state-specific rules impacted payouts. Payment breakdown modules provided contextual detail, replacing static documents with clear, structured explanations supported by visual hierarchy and hover-based detail where appropriate.
A unified claim status area consolidated key information in one place, reducing reliance on HR for interpretation. Documentation workflows were streamlined, enabling users to upload, view, and manage required materials directly within the system.
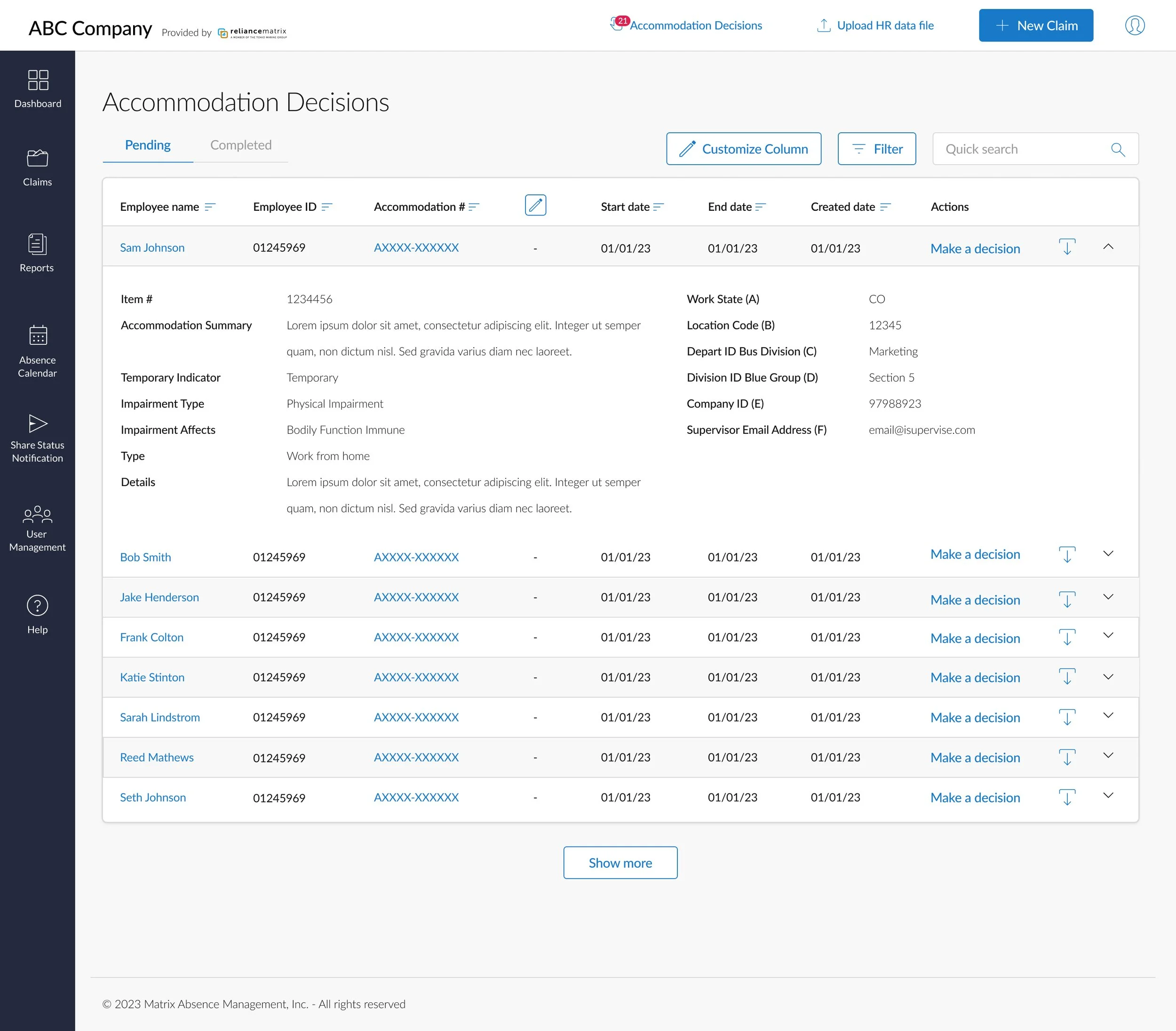
For employers, the experience expanded into a more capable administrative portal. Dashboards provided visibility into active claims, reporting tools, absentee tracking, and user management. Notifications and status updates were surfaced more clearly, improving operational oversight.
The result was a more transparent, compliant, and confidence-building experience that reduced ambiguity for employees while improving administrative efficiency for employers.